Neonatal Scrub Typhus: Case Report
Sunil Gothwal, Sneha Singh Dhruw, Ramesh Choudhry and Sitaraman S
Kaneda K1*, Kogaka S2, Yokyam SA3, Soga Y4 and Yonekura T2
1Department of Cardiovascular Surgery, School of Medicine, Nara Hospital, Kindai University, Otoda-cho, Ikoma, Nara 630-0293, Japan
2Department of Pediatric Surgery, School of Medicine, Nara Hospital, Kindai University, Otoda-cho, Ikoma, Nara 630- 0293, Japan
3Department of Thoracic and Cardiovascular Surgery, Nara Medical University, Shijo-cho, Kashihara, Nara 634-8522, Japan
4Department of Cardiovascular Surgery, Nagahama City Hospital, Ooinui-cho, Nagahama, Shiga 526-8580, Japan
- *Corresponding Author:
- Kozo Kaneda
Department of Cardiovascular Surgery, School of Medicine, Nara Hospital, Kindai University 1248-1, Otoda-cho, Ikoma, Nara 630-0293 Japan.
Tel: +81743770880
Fax: +81743770890
E-mail: kaneda_0117@yahoo.co.jp
Received date: March 14, 2016; Accepted date: April 19, 2016; Published date: April 22, 2016
Citation: Kaneda K, Kogaka S, Yokyam AS, et al. A Child with Acute Fulminant Myocarditis that Presented as Acute Abdomen. Pediatr Emerg Care Med Open Access. 2016, 1:2.
Abstract
Background: The clinical situation of patients with acute fulminant myocarditis can rapidly worsen dramatically, and a delayed diagnosis can lead to poor outcomes.
Objectives: To report a case of acute fulminant myocarditis with an extremely rare clinical course that was successfully treated. Case presentation: A 6-yearold girl was diagnosed with acute fulminant myocarditis during endoscopic cholecystectomy, requiring emergent percutaneous cardiopulmonary support.
Method: Initially, torsion of the gallbladder was suspected on abdominal computed tomography, and she underwent endoscopic abdominal cavity exploration. However, there was no inflammatory change in the abdominal cavity. Complete atrial ventricular block and a wide QRS wave were noted during closure of the trocar hole, and ventricular fibrillation occurred subsequently. Cardiopulmonary resuscitation was immediately initiated but was not effective. Emergent cardiopulmonary support was therefore introduced.
Results: Weaning from percutaneous cardiopulmonary support was performed at 8 days after the critical event. There was no cardiac dysfunction before hospital discharge. The patient has not experienced any critical symptoms at 3 years after recovery.
Conclusion: Abdominal symptoms in children might be related with acute fulminant myocarditis. If a child presents with any abdominal symptoms, special attention should be provided and the possibility of acute fulminant myocarditis should be considered.
Keywords
Fulminant myocarditis; Acute abdomen; Cardiopulmonary support; Child
Introduction
Acute fulminant myocarditis (AFM) in children is associated with several atypical symptoms as antecedent signs, such as low-grade fever, upper respiratory symptoms, abdominal pain, nausea, and vomiting. Therefore, it is difficult or impossible to obtain an early accurate diagnosis. A delayed diagnosis can be fatal or can result in poor outcomes. Here we report a child with AFM having an extremely rare clinical course, who we successfully treated. The child was diagnosed with AFM during endoscopic abdominal cavity exploration for acute abdomen, requiring emergent percutaneous cardiopulmonary support (PCPS).
Case
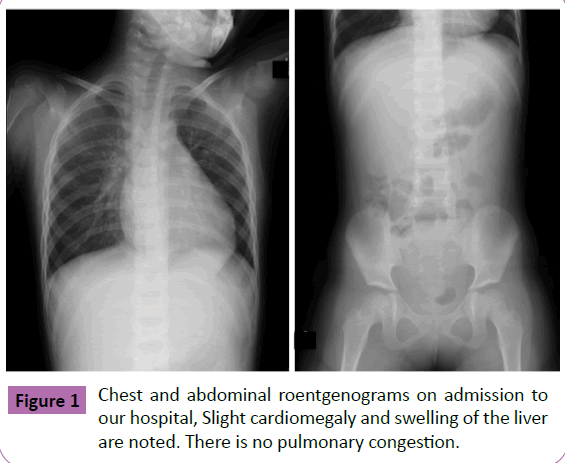
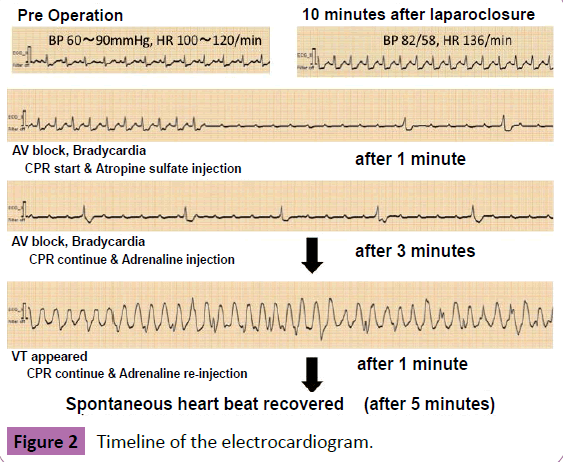
The patient was a 6-year-old girl who was referred to our hospital because of suspicion of acute cholecystitis. She had severe abdominal pain and vomiting. Cyanosis and respiratory distress were absent. Blood examination revealed moderate elevation of the transaminase level, moderate elevation of the creatine phosphokinase level, and mild elevation of the C-reactive protein level. However, the blood cell count was within the normal limit (Table 1). Preoperative chest radiography showed slight cardiomegaly and no pulmonary congestion (Figure 1). Computed tomography showed slight wall thickening of the gallbladder, without other abnormal findings. Hence, acute cholecystitis was excluded and torsion of the gallbladder was suspected. On emergent endoscopic abdominal cavity exploration, there was no inflammatory change in the abdominal cavity and the gallbladder was almost normal. However, the intestine was slightly edematous and pale. Closure of the trocar hole was performed; however, complete atrioventricular block occurred during wound closure. The QRS wave on an electrocardiogram (ECG) widened gradually, and ventricular tachycardia (VT) was noted subsequently. Cardiopulmonary resuscitation was immediately performed, but it was not effective (Figure 2).
Hematology |
Biochemical test |
||
|---|---|---|---|
| WBC | 6.85 (1CK/P I) | TWA protein | 5.6 (8/41) |
| RBC | 3.64 (10./P I) | Albumin | 33 (2/d1) |
| Hemoglobin | 10.2 (g/dI) | TWA bilirubin | 0.4 Osted1) |
| Hematocrit | 29.0 (%) | Direct bilirubin | 0.2 (mg/d1) |
| Platelet | 33.4 (10/P I) | AST | 709 (U/U |
| Neutrophile | 55.1 (%) | ALT | 603 (U/U |
| Lymphocyte | 40.1 (N) | LDH | 1136 (U/U |
| Menem,. | 4.7 (%) | Alkaliphosphatase 304 (U/U | |
| Eosinocyto | 0 (6) | Gamma GIP | 14 (U/L) |
| Basocoto | 0.1 (%) | CPK | 462 (U/U |
| Creatinine | 0.3 (mg/d1) | ||
| Coagulation system | BUN | 26.9 (mg/d1) | |
| PT sec | 15.7 (sec) | Glucose | 215 (mg/di) |
| PT-INR | 1.65 | Na | 130 (mEp/1-) |
| APTT | 28.5 (sec) | CI | 95 (mEcKL) |
| Fibrinogen | 205 (mg/d1) | K | 4.3 (mEq/1-) |
| FDP(pbasma) | 13.5 (0 g/m1) | CRP | 2.25 (mg/d0 |
Table 1: Blood examination results on admission to our hospital, Black, normal range; Blue, low value; Red, high value.
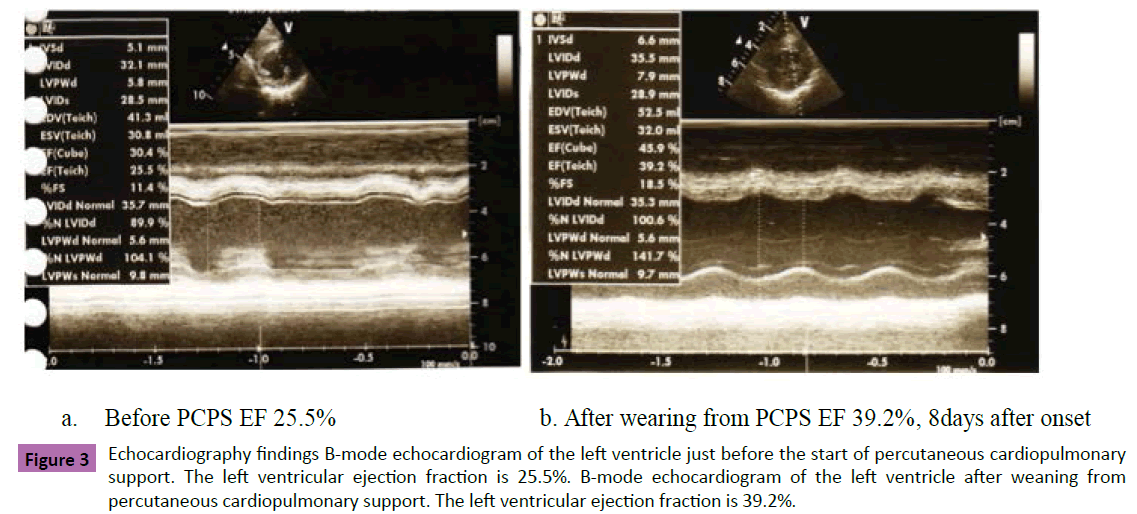
Echocardiography showed diffuse severe hypokinesis of the heart (Figure 3a). We noticed that these critical symptoms were induced by AFM. Emergent mechanical cardiopulmonary support (CPS) was necessary. Cardiovascular surgeons rushed to the operating room and decided to introduce a PCPS system.
Figure 3 Echocardiography findings B-mode echocardiogram of the left ventricle just before the start of percutaneous cardiopulmonary support. The left ventricular ejection fraction is 25.5%. B-mode chocardiogram of the left ventricle after weaning from percutaneous cardiopulmonary support. The left ventricular ejection fraction is 39.2%.
Cannulation was performed using Seldinger’s technique. An infusion cannula (12Fr) was inserted into the abdominal aorta through the left femoral artery, and a drainage cannula (14Fr) was inserted into the right atrium through the right femoral vein. A centrifugal pump was employed, and non-pulsatile flow was used. Initially, extracorporeal flow was set at 2.0 L/m2/min. After introduction of PCPS, her circulatory condition stabilized, and normal sinus rhythm was maintained without any arrhythmia. Because oliguria was observed, continuous hemodiafiltration was performed simultaneously. Fortunately, the ECD pattern improved, and the QRS wave normalized 2 days after initiation of PCPS. Weaning from PCPS was undertaken 8 days after the critical event. Diffuse severe hypokinesis was noted on echocardiography at the time of weaning from PCPS (Figure 3b). However, cardiac contractility recovered gradually. There was no cardiac dysfunction before hospital discharge. The patient has not experienced any clinical symptoms at 3 years after recovery.
Discussion
The clinical situation of patients with AFM can worsen dramatically in the short-term. The antecedent signs of this disease are associated with several atypical symptoms. Therefore, the precise diagnosis of AFM is usually delayed, resulting in poor outcome. Some patients with AFM might not be diagnosed after death. The mortality rate of patients with AFM reported in previous studies was based on the outcomes of patients who had been treated at eminent hospitals. Therefore, the accurate mortality rate of patients with AFM is unclear. According to 2 large studies that included over 20 patients, the requirement ratios for introduction of CPS for AFM are 32%, and 50%, and the ratios for weaning off from CPS are 63% and 70%, respectively. [1.2] Several previous articles on AFM have reported good clinical outcomes after recovery from severe cardiac dysfunction among patients who required mechanical CPS [1-5].
We have treated 4 patients with AFM using PCPS until date and all these patients were successfully weaned from PCPS (Table 2). All patients had prior abdominal symptoms, such as pain, and vomiting. The present patient had a unique clinical course. She was initially considered to have acute torsion of the gallbladder based on only abdominal symptoms, and therefore, she underwent endoscopic abdominal cavity exploration. Additionally, she had no obvious symptoms of acute heart failure preoperatively. This case suggests that AFM should be considered as a possible diagnosis in children with abdominal symptoms.
| Case | Age | Gender | Height | Weight | BSA | Upper Resp Symptom |
Abdominal Symptom |
Latent period (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | M | 75 | 10 | 0.44 | + | + | 3 |
| 2 | 13 | M | 140 | 30 | 1.1 | — | + | 3 |
| 3 | 14 | M | 168 | 60 | 1.68 | ±(flu A) | + | 35 ? |
| 4 | 6 | F | 112 | 17.5 | 0.74 | + | + | 14 |
Table 2 Characteristics of our patients with acute fulminant myocarditis, BSA, body surface area; Resp, respiratory; M, male; F, female; flu, influenza.
If CPS is required in children with AFM, the choice of the access point and cannula size is very important. In previous reports, an almost open chest approach was used, with a CPB flow of 1.2-1.8 L/min/m2 and CPS duration of 3-9 days. [1-3] All of our patients had been treated with the percutaneous approach. According to our experience, the percutaneous approach will be possible if body weight is more than 10 kg or body surface area is more than 0.45 m2. However, among our patients, 1 patient could not achieve sufficient pump flow owing to the presence of a small drainage cannula, and this patient experienced VT storm until exchange of the drainage cannula. Therefore, we considered that pump flow should be more than 2.0 L/min/m2 to maintain systemic perfusion and reduce myocardial workload. Additionally, our patients could be weaned from PCPS at around 7days, except 1 patient. The patient could be weaned from PCPS at 20 days. Unfortunately, the patient was complicated with large intracerebral bleeding. We considered that the criterion of weaning from CPS is normalization of the ECG, and normalization of left ventricular contraction on echo findings is not necessary. However, care should be taken, as prolonged CPS can lead to bleeding complications.
Conclusion
We reported a child with AFM having an extremely rare clinical course, who was successfully treated. If a child presents with any abdominal symptoms, special attention should be provided and the possibility of AFM should be considered. If CPS is introduced, it should be discontinued as soon as possible to avoid bleeding complications.
Financial Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- Kim KS, Ando K, Asakai H, Hayashi T, Kaneko M, et al. (2010) The prognosis of children with acute myocarditis in our institute where percutaneous cardiopulmonary support (PCPS) is available. Pediatr Cardiol Card Surg 26:227-233.
- Teele SA, Allen CK, Laussen PC, Newburger JW, Gauvreau K, et al. (2011) Management and outcomes in pediatric patients presenting with acute fulminant myocarditis. J Pediatr 158: 638-643.
- Kanamaru H, Karasawa K, Abe O, Miyashita M, Ayusawa M, et al. (2007) Recommendations for weaning off cardiopulmonary support in children with fulminant myocarditis. Circ J 71: 1551-1554.
- McCarthy RE 3rd, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, et al. (2000) Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med 342: 690-695.
- Asaumi Y, Yasuda S, Morii I, Kakuchi H, Otsuka Y, et al. (2005) Favourable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation. Eur Heart J 26: 2185-2192.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences