Drip Infusion Cholangiography with Computed Tomography in the Evaluation of Bile Leakage after Blunt Liver Trauma in Children: Two Case Reports
Otake K, Uchida K, Nagano Y, Noguchi T, Shimura T, Matsushita K, Inoue M and Kusunoki M
Department of Gastrointestinal and Pediatric Surgery, Mie University Graduate School of Medicine, Tsu, Mie, Japan
- *Corresponding Author:
- Kohei Otake
Department of Gastrointestinal and Pediatric Surgery
Mie University Graduate School of Medicine, 2-174 Edobashi
Tsu, Mie 514-8507
Japan
E-mail: kohei815@clin.medic.mie-u.ac.jp
Keiichi Uchida
Department of Gastrointestinal andPediatric Surgery
Mie University Graduate School of Medicine, 2-174 Edobashi
Tsu, Mie 514-8507
Japan
Tel: +81-59-232-1111 extn. 5645
Fax: +81-59-232-6968
E-mail:ucchie@clin.medic.mie-u.ac.jp
Received date:January 21, 2016; Accepted date: March 07, 2016; Published date: March 13, 2016
Citation: Otake K, Uchida K, Nagano Y, et al. Drip Infusion Cholangiography with Computed Tomography in the Evaluation of Bile Leakage after Blunt Liver Trauma in Children: Two Case Reports. Pediatr Emerg Care Med Open Access. 2016, 1:1.
Abstract
Bile duct injury following blunt liver injury is rare, and the precise site of bile leakage is often difficult to identify with noninvasive techniques. Endoscopic retrograde cholangiopancreatography is being used increasingly more often in the evaluation and management of biliary disorders in children. However, it is invasive and often requires general anesthesia in children. Drip infusion cholangiography with computed tomography (DIC-CT) is reportedly a noninvasive, safe way to diagnose and localize the site of bile leakage. We herein report two pediatric cases of bile leakage after blunt liver trauma in which DIC-CT was helpful in the case management decision-making process. DIC-CT could be a very powerful
Keywords
DIC-CT; Bile duct injury; Blunt liver trauma
Case Presentation
Case 1
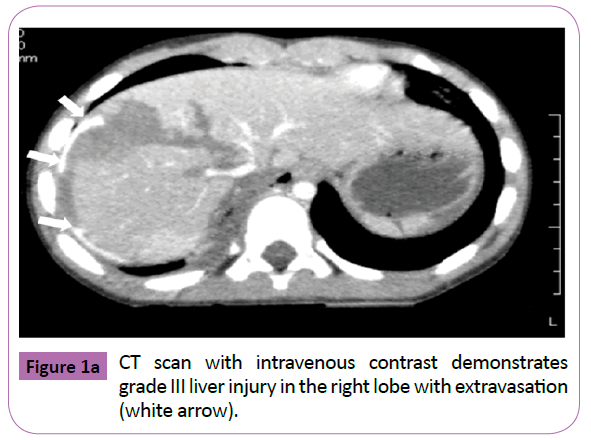
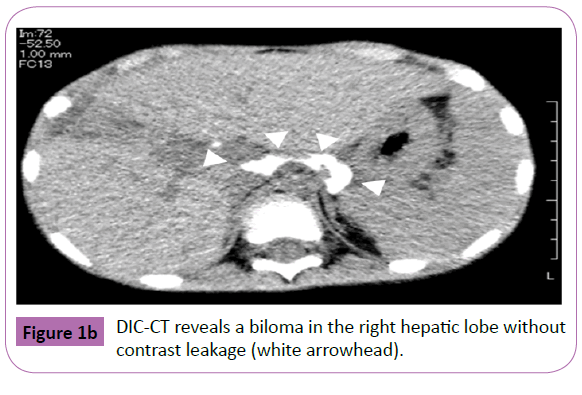
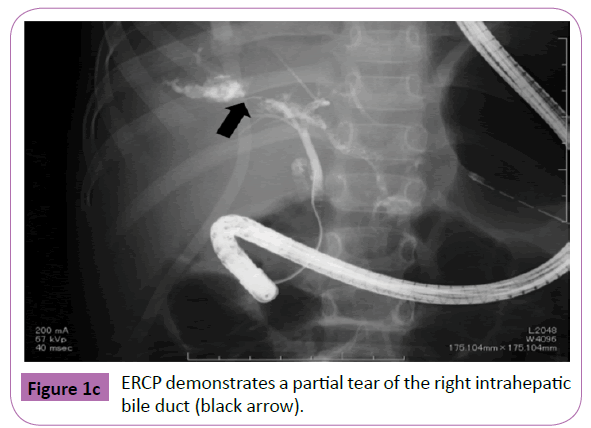
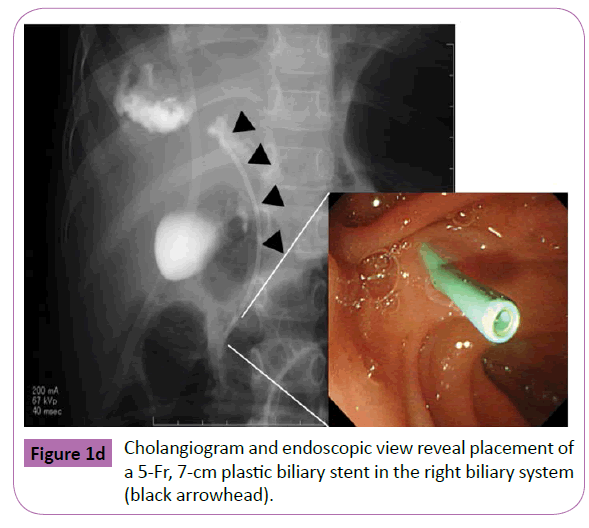
A 5 year old boy was admitted at the emergency room after having been run over by a car. He sustained bilateral hemopneumothorax, bilateral pulmonary contusion, right kidney injury, an unstable pelvic ring fracture, and a right femoral neck fracture. He was intubated and fluid resuscitation was commenced. Bilateral chest tubes were inserted because of hemopneumothorax. A CT scan with intravenous contrast revealed grade III injury in the right liver lobe (Figure 1a) and grade 3 injury of the right kidney. With the patient under general anesthesia, an interventional radiologist performed transcatheter arterial embolization (TAE) to embolize the injured hepatic and pelvic arteries. The anesthesiologist continued resuscitation throughout the embolization procedure. Extracorporeal membrane oxygenation was initiated because of severe respiratory failure on day 1 and weaned on day 5. The femoral neck fracture was repaired on day 17. The patient became jaundiced, and a CT scan showed the presence of free fluid in the left upper quadrant of the peritoneal cavity. An external drain placed under ultrasound guidance yielded bile-stained fluid. On day 25, drip infusion cholangiography with computed tomography (DICCT) (2 mL/kg body weight of meglumine iotroxate) clearly showed a right biliary duct injury and contrast leakage (Figure 1b). On day 44, therapeutic ERCP was performed under general anesthesia, because the bile-stained fluid from the peritoneal drain persisted.ERCP demonstrated a partial tear of the right intrahepatic bile duct (Figure 1c). A 5-Fr, 7-cm endoscopic retrograde biliary drainage tube was inserted across the ampulla (Figure 1d). The bile leakage was stopped, and the biliary drainage tube was removed on day 65. The peritoneal drain was removed on day 78. Follow-up ultrasound demonstrated no ascites or bile duct dilatation.
Case 2
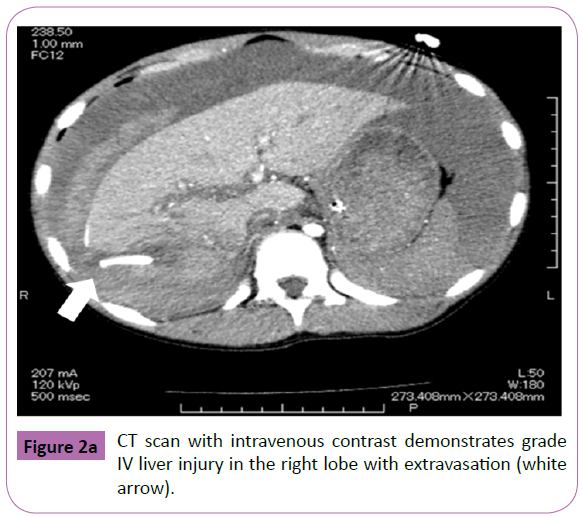
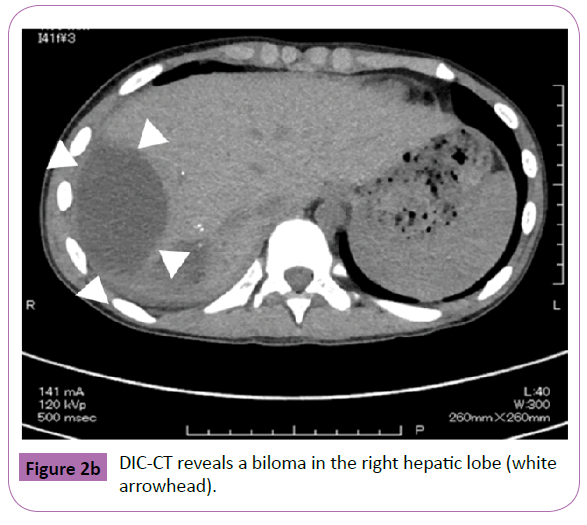
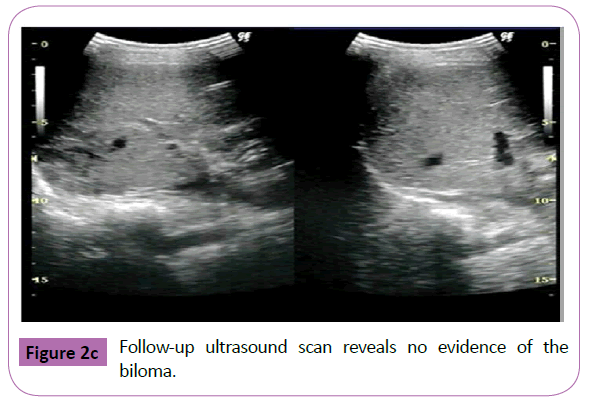
An 11-year-old girl was admitted to a local community hospital after having fallen nearly 2 m onto solid concrete. A CT scan of the abdomen with intravenous contrast revealed a liver laceration and small amount of free intraperitoneal blood. Fluid resuscitation was commenced, and she was transferred to our hospital. On arrival, she had a Glasgow coma score of 14, heart rate of 140 bpm, and blood pressure of 90/53 mmHg. However, her skin felt cool to the touch, and her capillary refill time was 5 seconds. Thus, a blood transfusion was initiated. A CT scan with intravenous contrast identified grade IV injury in the right liver lobe and a significant amount of abdominal free fluid with extravasation into the intraperitoneal cavity (Figure 2a). With the patient under general anesthesia, an interventional radiologist performed TAE to embolize the injured hepatic artery. The patient did well following TAE and was started on an oral diet; however, a follow-up ultrasound examination and CT scan on day 26 showed the development of a biloma in the right hepatic lobe. On day 27, DIC-CT (2 mL/kg body weight of meglumine iotroxate) showed no leakage (Figure 2b). The biloma was managed conservatively. On day 29, she was discharged uneventfully, and a follow-up ultrasound examination on an outpatient basis revealed normal findings (Figure 2c).
Discussion
Biliary complications following blunt liver injury have been reported in 2.8% to 7.4% of adults and 4.0% of children [1,2]. Accurate and early diagnosis is imperative, and imaging plays a key role in the management of bile leakage following blunt liver trauma. Hepatobiliary scintigraphy, contrast-enhanced magnetic resonance cholangiography, and diagnostic ERCP have been used to diagnose bile leakage. Hepatobiliary scintigraphy has poor spatial resolution and cannot localize the leakage site. Contrastenhanced magnetic resonance cholangiography requires a long period of time for opacification of the bile ducts; additionally, its contrast agent, gadobenate dimeglumine, has not been approved in some countries including Japan. ERCP and transhepatic cholangiography are the best techniques with which to visualize the biliary system. ERCP is being used increasingly more often in the evaluation and management of biliary and pancreatic disorders in children [3]. Additionally, the use of therapeutic ERCP with endobiliary stenting in the management of bile duct injuries after blunt liver trauma is well documented in adults, and several studies have also been reported in children [4]. However, ERCP is an invasive technique, and the need for general anesthesia is much more frequent in children than in adults. Hense, ERCP is rarely the first line choice for diagnosis of a suspected bile leak. DIC-CT is reportedly a noninvasive, safe technique with which to diagnose and localize the site of bile leakage in children [5,6]. Our technique of DIC-CT requires the intravenous administration of meglumine iotroxate (Biliscopin; Bayer Schering Pharma, Osaka,Japan) at a dose of 2 mL/kg body weight (maximum dose, 100 mL) for 30 min. CT data were acquired at 15 and 30 min after drip infusion of the contrast media without sedation. DIC-CT provides images with high spatial resolution in a short scanning time. The main disadvantages of DIC-CT include the possibility of adverse reactions to the biliary contrast media and insufficient depiction of the bile ducts caused by liver dysfunction or obstructive jaundice. Another disadvantage is that the market for intravenous contrast media of DIC-CT is limited to a few countries [7].
Bile duct injury such as that seen in Case 1 in the present report requires surgical intervention with some form of resection, which often is difficult and carries with it significant morbidity. DIC-CT revealed the precise site of biliary duct injury and leakage using a contrast agent. Because the bile leak was well drained and the child was asymptomatic, we performed therapeutic ERCP to allow for regeneration of the damaged hepatic tissue. ERCP and endobiliary stenting were successfully performed, and the child recovered uneventfully. In Case 2, CT revealed a delayed biloma in the right hepatic lobe, and DIC-CT showed no bile duct leakage. We therefore managed the biloma conservatively, and the child recovered uneventfully. DIC-CT obviated the need for ERCP in this case. In both cases, DIC-CT was a very powerful and much less invasive technique than ERCP or transhepatic cholangiography in an already damaged liver.
In conclusion, we report two pediatric cases of bile leakage after blunt liver trauma in which DIC-CT was helpful in the case management decision-making process. DIC-CT is technically feasible and safe in children and may help to noninvasively diagnose and localize the site of post-traumatic bile leakage in children. DIC-CT could allow for detailed evaluation of the biliary anatomy in a short scanning time and obviate the need for ERCP.
References
- Bala M, Gazalla SA, Faroja M, Bloom AI, Zamir G, et al. (2012) Complications of high grade liver injuries: management and outcomewith focus on bile leaks. Scandinavian journal of trauma, resuscitation and emergency medicine 20: 20.
- Kulaylat AN, Stokes AL, Engbrecht BW, McIntyre JS, Rzucidlo SE, et al. (2014) Traumatic bile leaks from blunt liver injury in children: a multidisciplinary and minimally invasive approach to management. Journal of pediatric surgery 49: 424-427.
- Enestvedt BK, Tofani C, Lee DY, Abraham M, Shah P, et al. (2013) Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. Journal of pediatric gastroenterology and nutrition 57: 649-654.
- Castagnetti M, Houben C, Patel S, Devlin J, Harrison P, et al. (2006) Minimally invasive management of bile leaks after blunt liver trauma in children. Journal of pediatric surgery 41: 1539-1544.
- Youngson GG, Driver CP, Mahomed AA, Duddalwar VA (2003) Computed tomographic cholangiography in the diagnosis of bile duct injury in children. Journal of pediatric surgery 38: E18-E20.
- Wicky S, Gudinchet F, Barghouth G, Schnyder P (1999) Three-dimensional cholangio-spiral CT demonstration of a post-traumatic bile leak in a child. European radiology 9: 99-102.
- Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, et al. (2012) CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. The British journal of radiology 85: 887-896.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences